Most of the time, Whitney Weldon doesn’t think about her second skeleton.
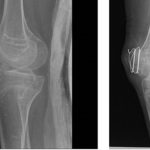
She was 9 the first time it really flared up. Bridges of bone grew from nowhere to freeze her right arm at a 120-degree angle, an excruciating experience that felt “like your bones are trying to come out of your skin,” she said. A decade later, her second skeleton sprouted struts of bone that locked the other arm in place, this time at 180 degrees. Weldon, then a high school senior, gave herself a month to accept that she could no longer drive, no longer put on a shirt without help. And then she started preparing for college.
“It’s all these new normals that you have to get used to,” said Weldon, now 27. “You have to grieve a part of you that you can no longer use. And then you have to move on.”
Weldon is one of about 800 people in the world with fibrodysplasia ossificans progressiva, or FOP. It’s a grim genetic disease in which the body’s machinery for healing goes awry, growing immovable bone where it doesn’t belong. Minor injuries can lead to debilitating inflammation that leaves limbs unusable. And even a life of caution can’t stop its progress. As time goes on, those second skeletons will gradually freeze joints in place with rigid sheets of bone, leaving patients unable to walk, speak, or breathe. The median life expectancy is about 55 years.
For decades, FOP was a medical curiosity, a disease without a treatment or even a biological explanation. But thanks to a well-organized patient group, some dedicated researchers, and a fair amount of scientific serendipity, the future of FOP could be unprecedentedly bright.
“It’s really a story about a community that came together to solve a problem,” said Dr. Fred Kaplan, an orthopedic surgeon-turned-geneticist at the University of Pennsylvania who is regarded as the godfather of FOP research. “And I truly believe this is a problem that will get solved.”
There are three medicines now in human trials, the most advanced of which could win Food and Drug Administration approval next year. A community once relegated to what Kaplan calls “the backwaters of medicine” now sees a future in which a cocktail of therapies might arrest unwanted bone growth and halt FOP.
“I never thought that this would even be a possibility,” said Weldon. “It would be a lot of happy tears, finding a medication.”
The history of FOP research is laden with chance encounters and unforgettable images, lives forever redirected after learning about the disease.
Kaplan’s conversion came in 1988. He had a cursory knowledge of FOP after treating a pair of adults in Philadelphia, but he didn’t understand the scope of the disease until a colleague introduced him to a little girl in North Carolina. The meeting would send him on a nearly two-decade quest to find the genetic mutation responsible.
“When you look at adults with FOP, it’s like going to the World Trade Center site and seeing the memorial there,” Kaplan said. “You can intellectualize that a terrible attack occurred there, but you have to close your eyes. But looking at a child where this is an ongoing process, it was like watching the planes fly into the building. It has a deep visceral effect.”
For Aris Economides, life changed the day he met Harry Eastlack. It was Aug. 30, 1996, and Economides, a researcher at Regeneron Pharmaceuticals just out of postdoctoral training, was spending his Saturday night leafing through the journal Science. There, on page 1,170 of Volume 273, was Eastlack.
Or, more precisely, his skeleton.
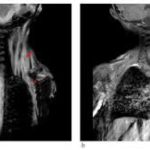
Eastlack’s neck was craned unnaturally to the side. His arms were creased at the elbow. His right knee bent awkwardly backward. And all over his skeleton, donated to science after his death in 1973, were expanses of bone Economides had never seen in any X-ray or diagram.
“I see this picture, and I say, ‘Oh, my God, what is this?’” Economides said. It was happenstance, but it would set in motion the next two decades of his work, which had already focused on the proteins that drive bone growth. A few blind alleys and fortunate discoveries later Regeneron has an IV infusion, now in human trials, that Economides believes could change the lives of FOP patients.
Clarissa Desjardins, a scientist and biotech entrepreneur, had a similar experience 15 years later while browsing Nature Medicine. On page 454, researchers from Thomas Jefferson University said they had discovered that a class of drugs once meant to treat lung disease could halt bone growth in mice bred to replicate the effects of FOP.
The drugs were orally administered and had already proved safe in human trials, meaning the process of licensing one and repurposing it for FOP could be swift and, if successful, lucrative. She founded a company, Clementia Pharmaceuticals, and acquired the rights to such a drug from Roche.
“What really motivated me was the horrific nature of the disease,” Desjardins said. “Reading the paper as a mother and realizing that such a disease existed, that flabbergasted me.”
The two medicines, from Regeneron and Clementia, take differing molecular paths to achieve the same goal: stop bone growth before it steals away bodily function.
FOP results from a mutation to a gene called ALK-2. When that gene is overactive, it sets in motion a cascade of interlocking proteins, forming cartilage that will eventually harden into unwanted bone. Clementa’s drug, called palovarotene, is meant to interrupt the middle part of that process, targeting a receptor key to cartilage formation.
In a 12-week study, patients who took palovarotene during FOP flare-ups saw about 70 percent less new bone growth than those on placebo. A larger trial testing a daily dose of palovarotene is underway, but the FDA agreed to consider approving Clementia’s drug for use during flare-ups based on the earlier data, and the company plans to submit it for potential approval later this year.
Regeneron’s therapy, garetosmab, acts earlier in the FOP process. In order for mutant ALK-2 to set off the chain reaction that ossifies joints, it must bind to a protein that controls bone growth. Digging into that process, scientists at Regeneron homed in on a molecular matchmaker called Activin A. In healthy patients, the protein keeps ALK-2 from misbehaving and growing bone. But in FOP, it gets hijacked from exactly the opposite purpose.
Blocking Activin A with an antibody like garetosmab, Regeneron concluded, could be a way to systemically prevent the FOP flare-ups that lead to bone formation. Last year, the company started a global clinical trial to test the theory, recruiting 40 adults with FOP.
A third drug, from Blueprint Medicines, goes one step up the chain. Called BLU-782, it’s a pill meant to mute ALK-2’s activity before it has the chance to bind to Activin A in the first place. Targeting the genetic mutation responsible for a disease seems obvious, but previous attempts to shut off ALK-2 ran into a simple problem: The mutant gene looks quite a bit like its DNA neighbors, meaning an imprecise drug would wreak havoc on patients by interrupting necessary processes.
“It’s a tough scientific hurdle,” said Kate Haviland, Blueprint’s chief operating officer. “But through hard work and significant chemistry, we were able to successfully design a molecule that is exquisitely selective for ALK-2.”
Last month, Blueprint started a safety study, administering BLU-782 to healthy volunteers, and the company plans to start dosing FOP patients next year.
Whether any of the medicines ultimately reaches FOP patients remains to be seen. But the fact that they exist — and that they work in different ways — sets up a best-case scenario that once seemed unimaginable.
“We have the potential to have a cocktail for FOP in the same way that there’s a cocktail for other diseases, like HIV,” said Dr. Robert Pignolo, an FOP expert at the Mayo Clinic in Minnesota. “As long as the mechanism of action is different, then there’s a possibility of combining treatments.”
The first sign is usually the toes.
Children born with FOP have short, crooked big toes. Soon come inexplicable lumps and swelling, often on the back or shoulders, that lead parents to call their pediatricians. What typically ensues is months of doctoral guesswork, as kids are bounced from specialist to specialist before someone draws the line to FOP.
That was the case for the Otto family. In 2012, after months of MRIs and blood tests, their daughter, Sienna, was diagnosed with FOP. She was 2.
Doctors told her parents, Rory and Eric, to simply enjoy their time with a child who might only live to the age of 20. They put padding on all the corners of their house, bought their toddler a small helmet, and did everything they could to keep Sienna from any injury that might exacerbate her condition.
“We wanted to keep her in bubble wrap,” Rory Otto said.
But things would change dramatically. The Ottos got involved with the International FOP Association, a patient group that began as a pen-pal club 30 years ago. Before the drug industry took any interest, about 80 percent of all FOP research funds came from the parents and families that make up IFOPA, according to Penn’s Kaplan. The group, once 11 people strong, has grown into a deeply interconnected global organization that has raised millions of dollars in the quest for a cure.
Source: Stat News